Repetitive Strain Injury. August 23, 2011
Posted by Joanna Wilson in Uncategorized.Tags: carpal tunnel syndrome, dupuytrens contracture, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, raynauds, repetitive strain injury, RICE, RICE Treatment, rotator cuff injury, rsi, shoulder bursitis, tendonitis, tennis elbow, writers cramp
add a comment
 Repetitive Strain Injury (RSI) is a general term to describe chronic pain in any part of your upper body caused by overuse. It commonly affects arms, elbows, wrists, hands, fingers, neck, shoulder and the upper back. It is caused by doing an activity repeatedly over a long period of time.
Repetitive Strain Injury (RSI) is a general term to describe chronic pain in any part of your upper body caused by overuse. It commonly affects arms, elbows, wrists, hands, fingers, neck, shoulder and the upper back. It is caused by doing an activity repeatedly over a long period of time.
The term RSI covers a number of muscoskeletal injuries such as
- tendonitis
- carpal tunnel syndrome
- tennis elbow
- rotator cuff syndrome
- dupuytrens contracture
- writer’s cramp
- bursitis
- Raynauds phenomenon
Symptoms will be dependent on the anatomy and diagnosis of your condition but may include; stiffness, tingling, sharp or dull ache, pain in the muscle or joints, numbness, weakness, cramp or swelling.
Initially symptoms may only be present when performing the task and improve on resting, this may last for several weeks , but without treatment, your symptoms will get progressively worse.
Diagnosis of your symptoms will be made by your G.P. Repetitive strain injury is categorised into two types – Type 1 is when the doctor can diagnose a recognised medical condition such as the above list. Type 2 is where the doctor cannot diagnose a specific medical condition usually because there are no specific symptoms just a feeling of pain.
There are numerous causes of RSI dependant on your job or location of the injury. Some causes include repetitive activities, doing an activity which involves force i.e. carrying of lifting heavy objects, poor posture, awkward working position or carrying out an activity for a long period of time without an adequate break. Other causes are cold temperatures, working with vibrating equipment and stress.
Treatment will also be dependent on diagnosis but generally R.I.C.E treatment will be the initial management. Rest for a few days then begin mobilising the joint on the advice of your G.P. or physiotherapist. Applying ice-packs or heat packs may help alleviate your symptoms and reduce any swelling. Elastic supports or a splint could be used on the wrist or the elbow to give support. Your doctor may prescribe anti inflammatory medication to help with pain relief. If you are on other medication or suffer from stomach problems or asthma medication on the advice of your doctor only.
After this treatment, physiotherapy will be recommended. They will give you advice on posture, exercises to strengthen or relax muscles and can also perform TENS, ultrasound and infrared sessions.
If your symptoms are work related, look at ways to improve your working life. Talk to your manager about your problems and they can carry out a risk assessment. This may report that you need a new chair or a different keyboard, or they may be able to accommodate a new role that will help to relieve your symptoms.
Gilmore’s Groin. August 9, 2011
Posted by Joanna Wilson in Uncategorized.Tags: football, football injuries, football injury, gilmores groin, groin pull, groin strain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading, sportsman hernia, sportsmens hernia
add a comment
 Gilmore’s Groin was identified by Consultant Surgeon Dr Jerry Gilmore in 1980. It is a condition involving long standing groin pain and is also known as a sportsman’s hernia although there is no hernia present. It is common in footballers and rugby players due to the movements of kicking and twisting. Injury occurs at the junction of the leg and torso. It involves the area called aponeurosis where the three abdominal muscles, internal oblique’s, external oblique’s and transversus abdominus, converge to form the inguinal ligament. The external oblique has an archway where blood vessels and nerves pass through. A groin muscle tear opens this archway, widening it, the internal oblique is pulled up and the transversus abdominus is left unsupported.
Gilmore’s Groin was identified by Consultant Surgeon Dr Jerry Gilmore in 1980. It is a condition involving long standing groin pain and is also known as a sportsman’s hernia although there is no hernia present. It is common in footballers and rugby players due to the movements of kicking and twisting. Injury occurs at the junction of the leg and torso. It involves the area called aponeurosis where the three abdominal muscles, internal oblique’s, external oblique’s and transversus abdominus, converge to form the inguinal ligament. The external oblique has an archway where blood vessels and nerves pass through. A groin muscle tear opens this archway, widening it, the internal oblique is pulled up and the transversus abdominus is left unsupported.
Symptoms include pain during sporting activities particularly twisting, turning, kicking and hip extension. This pain usually radiates to the abductor muscle region and occasionally into the testicles. The day following exertion the sufferer will complain of being sore and stiff and may find it difficult to rise from bed or get out of a car, or any activity involving rising from a low position. Coughing and sneezing will also increase pain.
Diagnosis is based on patient history and symptoms. At least a third of patients have a specific injury they can say is the cause of the pain but the rest is usually a gradual build up of wear and tear. The most notable clinical sign is the widening of the superficial inguinal ring on the affected side, which can be palpated. Once other groin related injuries are ruled out treatment for Gilmore’s Groin can begin.
Conservative treatment by a physiotherapist is usually commenced as pain allows. They will work on a program of exercises to stabilise and strengthen the muscles of the pelvic region. If conservative treatment fails to work, surgery is required to repair the damaged area and restore normal function. Following surgery a 4-6 week rehabilitation program with a physiotherapist will begin to increase strength and flexibility to pelvic muscles. During this period you will be encouraged to avoid twisting and turning movements to prevent aggravation of the repair.
In the past, this type of injury could have ended a sportsman career, but due to Gilmores identification of this specific injury, most are fit and able to continue with their sporting career.
Getting back in shape. July 12, 2011
Posted by Joanna Wilson in Uncategorized.Tags: body recovery course, getting back in shape, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, post pregnancy exercise, pregnancy
add a comment
 Finding out you’re pregnant may be the best news you’ve ever had. You may pore over the books to see how your baby is growing week by week, but how is it affecting your body? During pregnancy your body changes dramatically. Apart from the obvious baby bump, many parts of your body will be affected due to hormonal surges. Your breasts, bottom, thighs, feet and hands may swell; you may suffer from heartburn, indigestion and urinary urgency and your skin may change to be better or worse.
Finding out you’re pregnant may be the best news you’ve ever had. You may pore over the books to see how your baby is growing week by week, but how is it affecting your body? During pregnancy your body changes dramatically. Apart from the obvious baby bump, many parts of your body will be affected due to hormonal surges. Your breasts, bottom, thighs, feet and hands may swell; you may suffer from heartburn, indigestion and urinary urgency and your skin may change to be better or worse.
Ligaments soften during pregnancy to prepare the mother for birth, couple this with postural changes necessary to accommodate for weight gain due to your bump and back pain is a normal consequence along with neck ache, headaches, aching legs and undue fatigue.
Following the birth, getting back into shape after baby has arrived is often a concern for new mums. Don’t rush immediately into a strict exercise regime, even if you think you still look pregnant. Give your body time to recover and heal and definitely wait until you stop bleeding. Most midwives recommend you leave strenuous exercise until after your 6 week check especially if you have had a caesarian.
However, Pelvic floor exercises should be started as soon as you feel able, as these muscles are weaker than they used to be. This will help to stop incontinence and can be done anywhere and no one will know.
New mothers generally concentrate on weight loss and toning of stomach muscles to try to regain their pre-pregnancy body. However, core muscles need the most attention as these provide long term support to your whole body. Without strengthening these muscles, a mother may suffer from stress incontinence, poor posture and back pain. Many new mothers cannot afford to be out of action with back pain whilst trying to look after a new baby.
Remember when starting an exercise regime, your joints and ligaments are still pliable, making it easier to injure yourself by overdoing it and stretching too much.
There are body recovery courses available to new mums to enable them to return to their former shape and size. These courses concentrate on gradually strengthening core muscles, providing support for the pelvis and spine and improving posture. They also help to avoid problems further down the line and address issues such as separated tummy muscles, stress incontinence and back pain. These courses allow you to take your baby with you if necessary, and provide a safe environment for them providing they are not crawling.
Whatever you decide to do, pace yourself. It took nine months to gain the weight and change your body so it may take this long to regain your former figure.
Os Trigonum Syndrome June 28, 2011
Posted by Joanna Wilson in Uncategorized.Tags: ankle injury, ankle sprain, football, football injuries, football injury, os trigonum, os trigonum syndrome, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 Os trigonum is an extra bone that develops behind the talus (ankle bone). It is connected to the talus with a fibrous band. This bone is present from birth but does not fuse with the talus, and is not normally diagnosed until adolescence in approximately 10% of people.
Os trigonum is an extra bone that develops behind the talus (ankle bone). It is connected to the talus with a fibrous band. This bone is present from birth but does not fuse with the talus, and is not normally diagnosed until adolescence in approximately 10% of people.
This extra bone only causes problems if the affected foot is pointed downwards regularly, for example ballet dancers or footballers. When this bony prominence is crushed between the tibia and the heel bone, the tissue surrounding the os trigonum can become trapped leading to inflammation and swelling. This condition is known as os trigonum syndrome.
The symptoms include pain at the back of the ankle and tenderness over the ankle bone. The area to the front of the Achilles tendon can be painful to the touch and the bony prominence may be palpable. Pain will be present on pointing the foot downwards. Some swelling around the ankle area may be present.
The symptoms can present like an ankle or Achilles tendon problem, therefore diagnosis is made by x-ray where the extra bone will be evident.
Once the diagnosis of os trigonum syndrome is made, rest is advised. Continuing activity will only aggravate the condition. Ice should be applied every few hours, not directly to the skin but wrapped in a towel, to help with pain and reduce inflammation. Anti-inflammatory medication may be prescribed by your doctor if the pain is severe. Immobilisation by a walking boot to restrict ankle movement may also relieve symptoms.
Conservative treatment can work for the majority of cases. However if you are a professional athlete or symptoms are not relieved by the above treatment, surgery may be needed. During surgery, the os trigonum is removed completely. This will make no difference to the foot movement or stability as it is an accessory bone. A splint will need to be worn for two weeks following surgery. Following the splint removal an extensive course of physiotherapy will be required for 2-3 months to regain muscle strength, stability and full range of movement to the ankle and leg.
Acute Torticollis June 14, 2011
Posted by Joanna Wilson in Uncategorized.Tags: acute torticollis, back pain, neck pain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, shoulder injury, torticollis, whiplash, wry neck
add a comment
 Torticollis means twisted neck, also referred to as wry neck, is a medical term for a stiff neck. Acute torticollis begins suddenly, usually you wake up with it and the cause is often unknown. It can be attributed to sleeping in an awkward position, sleeping in a draft or spending time outdoors in the wind. It can last from 24-48 hours to up to 2-3 weeks.
Torticollis means twisted neck, also referred to as wry neck, is a medical term for a stiff neck. Acute torticollis begins suddenly, usually you wake up with it and the cause is often unknown. It can be attributed to sleeping in an awkward position, sleeping in a draft or spending time outdoors in the wind. It can last from 24-48 hours to up to 2-3 weeks.
The pain is caused by the muscles in the neck going into spasm. Often the pain affects only one side of the neck but can radiate into the head or the shoulder. The neck may feel stuck in one position or cause spine contortion whereupon the neck is twisted to the right or the left.
Resting for a day or two can initially be helpful if the pain is severe. Your G.P. will be able to diagnose your condition based on your symptoms but if they have any doubts as to the cause of your neck pain, further investigations i.e. an x-ray may be ordered to rule out any disc involvement. A cervical collar should not be used unless the symptoms are particularly severe, and not for more than a few days as it is best to try to keep the neck mobile.
Analgesia, anti-inflammatory medication or muscle relaxants may help with symptom relief under the guidance of a doctor. Following a days’ rest, beginning gentle exercises will help prevent the neck from stiffening up further. A physiotherapist can provide gentle message and mobilisation of the neck to relieve symptoms.
Heat or cold packs may also help to resolve any inflammation and relieve pain. Use a few times a day, never apply these directly to the skin, always wrap in a towel to prevent further injury.
A physiotherapist can also give advice to improve your posture to promote good spinal alignment to prevent further episodes of torticollis reoccurring. The use of a good supportive pillow can also help you sleep in the correct position. It may be advisable to avoid driving if possible at the start of your injury because the restrictions on the turning of the head would make it impossible to view your blind spot.
Hip Labral Tears. May 31, 2011
Posted by Joanna Wilson in Uncategorized.Tags: acetabular labral tear, football, football injuries, football injury, groin strain, hip labral tear, hip pain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 A hip labral tear involves the ring of soft elastic tissue, called the labrum, which follows the outside rim of the socket of the hip (acetabulum). This injury can also be known as an acetabular labral tear.
A hip labral tear involves the ring of soft elastic tissue, called the labrum, which follows the outside rim of the socket of the hip (acetabulum). This injury can also be known as an acetabular labral tear.
Almost 80% of labral tears have no direct cause but are a build up of repeated minor traumas during high impact sports, such as football or golf, or are attributed to wear and tear of the hip joint due to degeneration. Sudden major trauma to the hip joint can cause a labral tear but further injuries are usually sustained.
Symptoms are a locking, clicking or catching sensation deep within the hip joint and can be accompanied by sharp groin or anterior thigh pain. The pain may become worse with flexion of the hip. There may also be a feeling of giving way, stiffness and a decrease in the range of movement of the hip.
Diagnosis of this injury is particularly hard because x-rays, CT, MRI and ultrasound scans do not pick up this injury. Diagnosis is made with a MR arthrogram, a specialised MRI scan combined with an injection of dye into the hip joint will show a labral tear.
Initial treatment, if the symptoms are not too severe is rest followed by physiotherapy. A physiotherapist will give you exercises to maximise hip range of movement to increase strength and stability. Some people recover in a few weeks with conservative treatment. Analgesia and anti-inflammatory medication will help with the pain; take these on the advice of your G.P.
If conservative treatment is unsuccessful or the symptoms are severe, hip arthroscopy can be performed. It is becoming increasingly popular for the treatment of labral tears and can be performed as day surgery. During the procedure the tear is visualised and trimmed effectively removing the problem. After surgery, crutches may be used for 4 or 5 days, and once incisions have healed, physiotherapy will begin. A physiotherapist will help to mobilise the hip joint to increase range of movement and progress onto muscle strengthening exercises. A return to sport could take 2-3 months.
Achilles Tendinopathy. May 17, 2011
Posted by Joanna Wilson in Uncategorized.Tags: achilles tendinopathy, football injuries, football injury, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
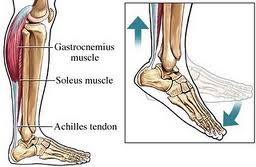 The Achilles tendon joins the heel bone (calcaneum) to the calf muscles. Its function is to flex the foot up and down. Formally referred to as Achilles tendonitis, Achilles tendinopathy is a more accurate name for this condition as it is now thought it is not an inflammatory condition.
The Achilles tendon joins the heel bone (calcaneum) to the calf muscles. Its function is to flex the foot up and down. Formally referred to as Achilles tendonitis, Achilles tendinopathy is a more accurate name for this condition as it is now thought it is not an inflammatory condition.
Achilles tendinopathy can be an acute or chronic condition. Acute conditions occur over a period of a few days and are usually a result of increase in activity, whereas chronic condition occurs over a longer period of time. Usually, degeneration of the tendon leads to decreased strength leading to injury. The condition can occur at the point of attachment to the heel or midway up the tendon and healing of the tendon is slow due to the poor blood supply.
The cause of Achilles tendinopathy is usually repeated tiny micro traumas to the tendon, followed by incomplete healing, occurring over time building up to injury. For example, overuse with excessive training, training in inappropriate footwear, spending a lot of your training running uphill, or constantly wearing high heels that shortens the Achilles tendon, then training in flat shoes causing excess strain on the tendon.
Achilles tendinopathy is more common in men than women, and more commonly occurs to those over 40. Symptoms begin gradually with pain at the back of the ankle especially when exercising, running uphill or climbing stairs. Pain will be worse in the morning or after a prolonged rest. The tendon will be tender on palpation and there may be some swelling and thickening of the tendon.
Diagnosis will be made by a doctor and you may have an ultrasound or MRI to rule out an Achilles tendon rupture. Self treatment will begin with R.I.C.E. Resting the foot will prevent further injury whilst applying ice and elevating the foot will help with swelling and pain. Ice should be wrapped in a towel before applying, do not apply ice directly to the skin. A compression bandage may help be giving support to the foot and ankle. Your G.P. may also prescribe painkillers to help alleviate symptoms. Always consult your doctor before taking medication to ensure they are suitable.
An extensive rehabilitation program will be recommended by your physiotherapist. The physio may use different techniques including massage, acupuncture, and ultrasound or taping. They will also recommend a series of stretching and strengthening exercises and advise of when to begin your training regime. It may take as long as 3 months to return to high impact sport. The physiotherapist will also observe your gait to assess if you have a mobility issue i.e. flat feet, which you may need an orthotic shoe insert to prevent increased pressure on your Achilles tendon.
Symptoms are usually gone in 3-6 months using these methods. If after this time you are still experiencing problems, there are other methods available but generally at the moment not on the NHS. These include extracorporeal shock-wave therapy, using sound waves to promote healing, Injection using autologous (your own) blood, which stimulates healing and using a glyceryl trinitrate patch for symptom relief and healing. These treatments are only recommended after a thorough consultation.
Approximately 1 in 4 people with Achilles tendinopathy will get no relief from any of the above and will need surgery. This usually removes nodules or adhesions on the tendon and a rehab program by a physiotherapist will follow post-op.
Facet Syndrome May 3, 2011
Posted by Joanna Wilson in Uncategorized.Tags: back pain, facet joint syndrome, facet joints, facet syndrome, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 Facet joints, also known as zygoapophyseal joints, are sections of the spine where vertebrae connect to one another. Facet joints allow a variety of movements for each vertebral level providing strength, flexibility and integrity to the spine.
Facet joints, also known as zygoapophyseal joints, are sections of the spine where vertebrae connect to one another. Facet joints allow a variety of movements for each vertebral level providing strength, flexibility and integrity to the spine.
Facet pain is chronic in nature and underlying causes are due to long term changes i.e. degenerative disc disease or osteoarthritis. Gymnasts and acrobats can also be prone to this type of injury due to the rigors of their sport.
Symptoms include severe spinal pain especially when moving and stiffness and limited motion. The pain will be worse when bending backwards or straightening back. If the facet syndrome affects the lumbar area, referred pain will be felt in the buttock, groin and thigh and down the sciatic nerve.
Diagnosis of facet syndrome is made by your G.P. or physiotherapist and you may be required to have an x-ray or MRI to confirm your specific condition.
Initially, treatment will be rest, but only for a short period. Physiotherapy will be encouraged as soon as possible. Your G.P. will probably advise anti-inflammatory medication depending on your past medical history.
A physiotherapist will help to improve and maintain flexibility and range of movement. They can also advise you on posture correction to relieve symptoms. Your physio may also perform acupuncture or, in severe cases, perform manipulation and spinal rotation. They may also advise you to use heat packs to relieve pain and muscle spasm. Always be careful when using heat therapy not to burn your skin. If physiotherapy alone does not work for you, you may be sent for a corticosteroid injection under radiography to help with pain relief.
Good posture can help prevent this condition and avoiding prolonged sitting or bending posture. See your local physiotherapist about good posture techniques for a healthy spine.
Headache relief. April 19, 2011
Posted by Joanna Wilson in Uncategorized.Tags: headache relief, Headaches, neck injuries, neck sprain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading
add a comment
 A headache is a pain or discomfort in the head or neck and is very common. Most of us experience some form of headache through a combination of every day factors, in particular dehydration, tiredness and poor posture. Headaches can also be brought on by stress.
A headache is a pain or discomfort in the head or neck and is very common. Most of us experience some form of headache through a combination of every day factors, in particular dehydration, tiredness and poor posture. Headaches can also be brought on by stress.
Less commonly are headaches that are chronic and persistent caused by meningitis, sinus and ear infections or anything more serious. However, if your GP can’t attribute your headache to something serious you may be suffering from an imbalance somewhere else in your body that might not be an immediately obvious cause of headaches.
Stress headaches are felt like a constant ache on both sides of the head and can cause tightening in the neck muscles. They are more common in women than men and can last from an hour to several days. If you have tried everything else, you could benefit from an appointment with a physiotherapist.
A common complaint is a feeling of tension in the head, which can sometimes be attributed to neck pain. This may be caused by something as simple as poor posture leading to tightness in the upper part of your spine and poor muscle action in and around the hips, perhaps by sitting badly or for too long at your desk or constantly carrying a heavy handbag on one side.
Many headaches are associated with neck pain. If your headaches are focused down one side of your head and worsened by movement of the neck, then it may be you are suffering from cervicogenic headache. Simply put, this means that the joints and muscles in your neck are restricted or tight and your physiotherapist can develop an appropriate programme of treatment to mobilise the area.
Persistent use of a mouse and crossing your legs when sitting can cause lengthening of certain muscles which results in a muscle imbalance and can lead to restricted joints and movement.
The good news is that many chronic headache conditions are often treatable through physiotherapy. The most important thing is to undergo a thorough assessment to see if your physiotherapist can identify a potential cause of your headaches.
Shoulder Bursitis. April 5, 2011
Posted by Joanna Wilson in Uncategorized.Tags: Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, shoulder bursitis, shoulder pain, Sporting injury, sports injury reading, tennis injury, volleyball injury
2 comments
 A bursa is a tiny fluid filled sac that acts as a gliding surface to reduce friction between tissues of the body. There are 160 bursae in the body located in the large joints, for example, knees, hips and shoulders. The bursa in the shoulder is located in-between the four muscles that make up the rotator cuff and the arch of the subacromial space, providing it with its name, subacromial bursa.
A bursa is a tiny fluid filled sac that acts as a gliding surface to reduce friction between tissues of the body. There are 160 bursae in the body located in the large joints, for example, knees, hips and shoulders. The bursa in the shoulder is located in-between the four muscles that make up the rotator cuff and the arch of the subacromial space, providing it with its name, subacromial bursa.
Bursitis is an inflammation of a bursa caused by injury or less commonly, infection. Shoulder bursitis is caused by repeated overhead movements causing the bursa to be squashed or impinged between the muscles and bones. A short spell of sport, where overhead movement is involved i.e. volleyball, when you are not used to it can cause bursitis.
Symptoms can come on gradually or be instantaneous. Localised pain or swelling, tenderness and pain with motion of the joint will indicate that you have a problem. Pain will be located at the tip of the shoulder and can radiate down the arm. You will not be able to raise your arm over your head. Pain can become worse if you lie on the affected side at night.
Diagnosis will be made by your G.P. or physiotherapist. An x-ray or MRI may be needed for diagnosis, to rule out other causes of the pain i.e. rotator cuff tear.
Treatment will depend on how far the bursa has developed. If it has just started, physical therapy can cause improvement. Ice therapy will be recommended by your physiotherapist, for 20 minutes every few hours. Never put ice directly on the skin, always wrap in a towel. This will reduce pain and inflammation along with resting the joint. Anti-inflammatory medication will help with the pain, under the supervision of your G.P.
A physiotherapist will then give you exercises to restore range of movement and increase muscle strength and stability. These may begin quite gently as pain allows but will build up to resistance exercises using a resistance band.
Occasionally these treatments will not reduce your bursa and a doctor will be required to drain it with a syringe in sterile conditions. You will then begin your physiotherapy as explained above.