Gilmore’s Groin. August 9, 2011
Posted by Joanna Wilson in Uncategorized.Tags: football, football injuries, football injury, gilmores groin, groin pull, groin strain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading, sportsman hernia, sportsmens hernia
add a comment
 Gilmore’s Groin was identified by Consultant Surgeon Dr Jerry Gilmore in 1980. It is a condition involving long standing groin pain and is also known as a sportsman’s hernia although there is no hernia present. It is common in footballers and rugby players due to the movements of kicking and twisting. Injury occurs at the junction of the leg and torso. It involves the area called aponeurosis where the three abdominal muscles, internal oblique’s, external oblique’s and transversus abdominus, converge to form the inguinal ligament. The external oblique has an archway where blood vessels and nerves pass through. A groin muscle tear opens this archway, widening it, the internal oblique is pulled up and the transversus abdominus is left unsupported.
Gilmore’s Groin was identified by Consultant Surgeon Dr Jerry Gilmore in 1980. It is a condition involving long standing groin pain and is also known as a sportsman’s hernia although there is no hernia present. It is common in footballers and rugby players due to the movements of kicking and twisting. Injury occurs at the junction of the leg and torso. It involves the area called aponeurosis where the three abdominal muscles, internal oblique’s, external oblique’s and transversus abdominus, converge to form the inguinal ligament. The external oblique has an archway where blood vessels and nerves pass through. A groin muscle tear opens this archway, widening it, the internal oblique is pulled up and the transversus abdominus is left unsupported.
Symptoms include pain during sporting activities particularly twisting, turning, kicking and hip extension. This pain usually radiates to the abductor muscle region and occasionally into the testicles. The day following exertion the sufferer will complain of being sore and stiff and may find it difficult to rise from bed or get out of a car, or any activity involving rising from a low position. Coughing and sneezing will also increase pain.
Diagnosis is based on patient history and symptoms. At least a third of patients have a specific injury they can say is the cause of the pain but the rest is usually a gradual build up of wear and tear. The most notable clinical sign is the widening of the superficial inguinal ring on the affected side, which can be palpated. Once other groin related injuries are ruled out treatment for Gilmore’s Groin can begin.
Conservative treatment by a physiotherapist is usually commenced as pain allows. They will work on a program of exercises to stabilise and strengthen the muscles of the pelvic region. If conservative treatment fails to work, surgery is required to repair the damaged area and restore normal function. Following surgery a 4-6 week rehabilitation program with a physiotherapist will begin to increase strength and flexibility to pelvic muscles. During this period you will be encouraged to avoid twisting and turning movements to prevent aggravation of the repair.
In the past, this type of injury could have ended a sportsman career, but due to Gilmores identification of this specific injury, most are fit and able to continue with their sporting career.
Os Trigonum Syndrome June 28, 2011
Posted by Joanna Wilson in Uncategorized.Tags: ankle injury, ankle sprain, football, football injuries, football injury, os trigonum, os trigonum syndrome, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 Os trigonum is an extra bone that develops behind the talus (ankle bone). It is connected to the talus with a fibrous band. This bone is present from birth but does not fuse with the talus, and is not normally diagnosed until adolescence in approximately 10% of people.
Os trigonum is an extra bone that develops behind the talus (ankle bone). It is connected to the talus with a fibrous band. This bone is present from birth but does not fuse with the talus, and is not normally diagnosed until adolescence in approximately 10% of people.
This extra bone only causes problems if the affected foot is pointed downwards regularly, for example ballet dancers or footballers. When this bony prominence is crushed between the tibia and the heel bone, the tissue surrounding the os trigonum can become trapped leading to inflammation and swelling. This condition is known as os trigonum syndrome.
The symptoms include pain at the back of the ankle and tenderness over the ankle bone. The area to the front of the Achilles tendon can be painful to the touch and the bony prominence may be palpable. Pain will be present on pointing the foot downwards. Some swelling around the ankle area may be present.
The symptoms can present like an ankle or Achilles tendon problem, therefore diagnosis is made by x-ray where the extra bone will be evident.
Once the diagnosis of os trigonum syndrome is made, rest is advised. Continuing activity will only aggravate the condition. Ice should be applied every few hours, not directly to the skin but wrapped in a towel, to help with pain and reduce inflammation. Anti-inflammatory medication may be prescribed by your doctor if the pain is severe. Immobilisation by a walking boot to restrict ankle movement may also relieve symptoms.
Conservative treatment can work for the majority of cases. However if you are a professional athlete or symptoms are not relieved by the above treatment, surgery may be needed. During surgery, the os trigonum is removed completely. This will make no difference to the foot movement or stability as it is an accessory bone. A splint will need to be worn for two weeks following surgery. Following the splint removal an extensive course of physiotherapy will be required for 2-3 months to regain muscle strength, stability and full range of movement to the ankle and leg.
Hip Labral Tears. May 31, 2011
Posted by Joanna Wilson in Uncategorized.Tags: acetabular labral tear, football, football injuries, football injury, groin strain, hip labral tear, hip pain, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 A hip labral tear involves the ring of soft elastic tissue, called the labrum, which follows the outside rim of the socket of the hip (acetabulum). This injury can also be known as an acetabular labral tear.
A hip labral tear involves the ring of soft elastic tissue, called the labrum, which follows the outside rim of the socket of the hip (acetabulum). This injury can also be known as an acetabular labral tear.
Almost 80% of labral tears have no direct cause but are a build up of repeated minor traumas during high impact sports, such as football or golf, or are attributed to wear and tear of the hip joint due to degeneration. Sudden major trauma to the hip joint can cause a labral tear but further injuries are usually sustained.
Symptoms are a locking, clicking or catching sensation deep within the hip joint and can be accompanied by sharp groin or anterior thigh pain. The pain may become worse with flexion of the hip. There may also be a feeling of giving way, stiffness and a decrease in the range of movement of the hip.
Diagnosis of this injury is particularly hard because x-rays, CT, MRI and ultrasound scans do not pick up this injury. Diagnosis is made with a MR arthrogram, a specialised MRI scan combined with an injection of dye into the hip joint will show a labral tear.
Initial treatment, if the symptoms are not too severe is rest followed by physiotherapy. A physiotherapist will give you exercises to maximise hip range of movement to increase strength and stability. Some people recover in a few weeks with conservative treatment. Analgesia and anti-inflammatory medication will help with the pain; take these on the advice of your G.P.
If conservative treatment is unsuccessful or the symptoms are severe, hip arthroscopy can be performed. It is becoming increasingly popular for the treatment of labral tears and can be performed as day surgery. During the procedure the tear is visualised and trimmed effectively removing the problem. After surgery, crutches may be used for 4 or 5 days, and once incisions have healed, physiotherapy will begin. A physiotherapist will help to mobilise the hip joint to increase range of movement and progress onto muscle strengthening exercises. A return to sport could take 2-3 months.
Achilles Tendinopathy. May 17, 2011
Posted by Joanna Wilson in Uncategorized.Tags: achilles tendinopathy, football injuries, football injury, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
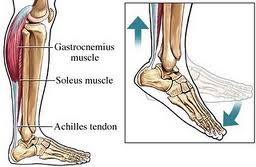 The Achilles tendon joins the heel bone (calcaneum) to the calf muscles. Its function is to flex the foot up and down. Formally referred to as Achilles tendonitis, Achilles tendinopathy is a more accurate name for this condition as it is now thought it is not an inflammatory condition.
The Achilles tendon joins the heel bone (calcaneum) to the calf muscles. Its function is to flex the foot up and down. Formally referred to as Achilles tendonitis, Achilles tendinopathy is a more accurate name for this condition as it is now thought it is not an inflammatory condition.
Achilles tendinopathy can be an acute or chronic condition. Acute conditions occur over a period of a few days and are usually a result of increase in activity, whereas chronic condition occurs over a longer period of time. Usually, degeneration of the tendon leads to decreased strength leading to injury. The condition can occur at the point of attachment to the heel or midway up the tendon and healing of the tendon is slow due to the poor blood supply.
The cause of Achilles tendinopathy is usually repeated tiny micro traumas to the tendon, followed by incomplete healing, occurring over time building up to injury. For example, overuse with excessive training, training in inappropriate footwear, spending a lot of your training running uphill, or constantly wearing high heels that shortens the Achilles tendon, then training in flat shoes causing excess strain on the tendon.
Achilles tendinopathy is more common in men than women, and more commonly occurs to those over 40. Symptoms begin gradually with pain at the back of the ankle especially when exercising, running uphill or climbing stairs. Pain will be worse in the morning or after a prolonged rest. The tendon will be tender on palpation and there may be some swelling and thickening of the tendon.
Diagnosis will be made by a doctor and you may have an ultrasound or MRI to rule out an Achilles tendon rupture. Self treatment will begin with R.I.C.E. Resting the foot will prevent further injury whilst applying ice and elevating the foot will help with swelling and pain. Ice should be wrapped in a towel before applying, do not apply ice directly to the skin. A compression bandage may help be giving support to the foot and ankle. Your G.P. may also prescribe painkillers to help alleviate symptoms. Always consult your doctor before taking medication to ensure they are suitable.
An extensive rehabilitation program will be recommended by your physiotherapist. The physio may use different techniques including massage, acupuncture, and ultrasound or taping. They will also recommend a series of stretching and strengthening exercises and advise of when to begin your training regime. It may take as long as 3 months to return to high impact sport. The physiotherapist will also observe your gait to assess if you have a mobility issue i.e. flat feet, which you may need an orthotic shoe insert to prevent increased pressure on your Achilles tendon.
Symptoms are usually gone in 3-6 months using these methods. If after this time you are still experiencing problems, there are other methods available but generally at the moment not on the NHS. These include extracorporeal shock-wave therapy, using sound waves to promote healing, Injection using autologous (your own) blood, which stimulates healing and using a glyceryl trinitrate patch for symptom relief and healing. These treatments are only recommended after a thorough consultation.
Approximately 1 in 4 people with Achilles tendinopathy will get no relief from any of the above and will need surgery. This usually removes nodules or adhesions on the tendon and a rehab program by a physiotherapist will follow post-op.
Facet Syndrome May 3, 2011
Posted by Joanna Wilson in Uncategorized.Tags: back pain, facet joint syndrome, facet joints, facet syndrome, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 Facet joints, also known as zygoapophyseal joints, are sections of the spine where vertebrae connect to one another. Facet joints allow a variety of movements for each vertebral level providing strength, flexibility and integrity to the spine.
Facet joints, also known as zygoapophyseal joints, are sections of the spine where vertebrae connect to one another. Facet joints allow a variety of movements for each vertebral level providing strength, flexibility and integrity to the spine.
Facet pain is chronic in nature and underlying causes are due to long term changes i.e. degenerative disc disease or osteoarthritis. Gymnasts and acrobats can also be prone to this type of injury due to the rigors of their sport.
Symptoms include severe spinal pain especially when moving and stiffness and limited motion. The pain will be worse when bending backwards or straightening back. If the facet syndrome affects the lumbar area, referred pain will be felt in the buttock, groin and thigh and down the sciatic nerve.
Diagnosis of facet syndrome is made by your G.P. or physiotherapist and you may be required to have an x-ray or MRI to confirm your specific condition.
Initially, treatment will be rest, but only for a short period. Physiotherapy will be encouraged as soon as possible. Your G.P. will probably advise anti-inflammatory medication depending on your past medical history.
A physiotherapist will help to improve and maintain flexibility and range of movement. They can also advise you on posture correction to relieve symptoms. Your physio may also perform acupuncture or, in severe cases, perform manipulation and spinal rotation. They may also advise you to use heat packs to relieve pain and muscle spasm. Always be careful when using heat therapy not to burn your skin. If physiotherapy alone does not work for you, you may be sent for a corticosteroid injection under radiography to help with pain relief.
Good posture can help prevent this condition and avoiding prolonged sitting or bending posture. See your local physiotherapist about good posture techniques for a healthy spine.
Acromioclavicular (AC) Joint separation. January 25, 2011
Posted by Joanna Wilson in Uncategorized.Tags: ac joint, ac joint separation, football injuries, football injury, Phsyiotherapy, physiocare, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
 A shoulder separation or acromioclavicular joint (AC) separation is a common sports injury, not to be mistaken with a shoulder dislocation as these are two different types of injury. A shoulder separation is caused by direct contact, for example, in rugby, or by landing on your shoulder, elbow or outstretched arm. The AC joint is the connection between the acromion of the scapula (shoulder blade) and the end of the clavicle (collar bone). The two bones are attached by the AC ligament but injuries can involve other ligaments i.e. the coracoclavicular (CC) ligament which joins the clavicle to the coracoid process, another protrusion on the scapula. The ligaments surround and support the AC joint forming the joint capsule.
A shoulder separation or acromioclavicular joint (AC) separation is a common sports injury, not to be mistaken with a shoulder dislocation as these are two different types of injury. A shoulder separation is caused by direct contact, for example, in rugby, or by landing on your shoulder, elbow or outstretched arm. The AC joint is the connection between the acromion of the scapula (shoulder blade) and the end of the clavicle (collar bone). The two bones are attached by the AC ligament but injuries can involve other ligaments i.e. the coracoclavicular (CC) ligament which joins the clavicle to the coracoid process, another protrusion on the scapula. The ligaments surround and support the AC joint forming the joint capsule.
Symptoms are immediate and can be severe. These include pain at the end of the clavicle, swelling and bruising. A step deformity may be visible. Pain may be felt when moving the shoulder especially when trying to raise the arm above shoulder height.
Diagnosis of this type of injury will be made after x-ray rules out any fractures to the bones around the shoulder. AC joint injuries are graded into six categories according to severity.
- Grade one is an injury to the capsule that surrounds the AC joint. The bones of the shoulder are not out of position
- Grade two is an injury to the capsule and ligaments that stabilise the clavicle.
- Grade three is the same as grade two but more significant. There will be a large bump over the injury.
- Grade four is an unusual injury. The clavicle is pushed behind the AC joint.
- Grade 5 is an exaggerated type of grade three. The muscle above the AC joint is punctured by the clavicle.
- Grade six is rare. The clavicle is pushed down and is lodged below the coracoid of the scapula.
Treatment initially is by the R.I.C.E. method. Rest the shoulder and apply ice frequently. This will help to reduce the swelling. The injury may be taped for two-to three weeks and immobilised in a sling. Anti-inflammatory medication may help will the pain at the advice of your doctor.
A physiotherapist will have a number of methods to help with symptom relief and rehabilitation. Ultrasound may be used on a minor injury or if the injury is more severe a TENS machine may help. Range of movement exercises should be started when pain eases followed by a program of strengthening exercises. A physiotherapist will advise you on the best exercise techniques for a speedier recovery. Surgery may be required for grades 4,5, and 6 but these are the most uncommon type of injury.
Colles Fracture December 28, 2010
Posted by Joanna Wilson in Uncategorized.Tags: colles fracture, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading, wrist sprain
add a comment
 With the increasing bad weather throughout the country, the chances of falling, especially for the unsteady or elderly, become more prevalent. A slip on the ice can lead to several injuries, one of which being a Colles fracture. A Colles fracture is a fracture of the radius bone of the forearm, just above the wrist, and is caused by falling with an outstretched arm. This type of fracture is named after Abraham Colles, an Irish surgeon who noted the symptoms of this fracture in 1814 before the use of x-ray.
With the increasing bad weather throughout the country, the chances of falling, especially for the unsteady or elderly, become more prevalent. A slip on the ice can lead to several injuries, one of which being a Colles fracture. A Colles fracture is a fracture of the radius bone of the forearm, just above the wrist, and is caused by falling with an outstretched arm. This type of fracture is named after Abraham Colles, an Irish surgeon who noted the symptoms of this fracture in 1814 before the use of x-ray.
Symptoms are felt immediately and include pain, tenderness, bruising and swelling. The wrist may also be bent into what is known as the ‘dinner fork’ deformity. If a fracture is suspected, a trip to accident and emergency is required. An x-ray will be performed to confirm diagnosis.
The severity of the injury will determine treatment. Initially, ice will be applied to help reduce swelling. If the fracture is well aligned and the bones are close, the wrist will be immobilised in a cast for about 6 weeks. The arm should be elevated to help reduce swelling. Once in a cast, finger sensation and colour should be observed. If the cast becomes very tight, the fingers become dusky coloured or there is any loss in sensation to the fingers, medical attention should be seeked immediately.
If the x-ray shows the fracture to be undisplaced and unaligned, the wrist will have to be manipulated into position. This will be done under anaesthetic and then put in a plaster cast for 6 weeks and the treatment then continues the same as non-surgical intervention.
During the period in plaster, rehabilitation exercises will be given by a physiotherapist to prevent stiffness in shoulder and elbow joints and you will be encouraged to wiggle your fingers regularly. After the six weeks in plaster, rehabilitation of the wrist and forearm muscles will begin. A physiotherapist will give you stretching and strengthening exercises for the wrist muscles to rebuild them up after being encased in plaster. A wrist brace may be provided for the first few weeks to wear in-between exercises until the wrist is stronger.
Sprained Ankle. December 14, 2010
Posted by Joanna Wilson in Uncategorized.Tags: ankle sprain, football, football injuries, football injury, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, Sporting injury, sporting injury reading, Sports injury, sports injury reading, sprained ankle
add a comment
 One of the most common orthopaedic injuries is a sprained ankle. It can happen during sporting activities or during everyday activities. It occurs following a sudden sideways twist of the foot or landing on an uneven surface. It is caused by injury to the ligaments of the ankle where they become partially or completely torn.
One of the most common orthopaedic injuries is a sprained ankle. It can happen during sporting activities or during everyday activities. It occurs following a sudden sideways twist of the foot or landing on an uneven surface. It is caused by injury to the ligaments of the ankle where they become partially or completely torn.
An inversion sprain is caused by the foot twisting inwards stretching one of the three lateral ligaments too far and account for about 90% of ankle sprains. The other 10% is caused by an eversion sprain where the foot is twisted outwards causing the medial ligament to be stretched.
Sprains are graded into three categories, mild, moderate and severe. Grade 1 is a mild stretch of the ligament and causes minimal pain and swelling. Grade 2 is a partial tear to the ligament causing moderate to severe pain, swelling and some bruising and some instability to the ankle joint. Grade 3 is a complete tear to the ligament causing severe pain, extensive swelling and bruising and the inability to weight bear. Other symptoms include the sensation of the ankle giving way and a popping sound heard at the time of injury.
Initially treatment should be by the R.I.C.E. method. Rest the ankle for 48-72 hours avoiding physical activity. Apply ice packs wrapped in a towel for 20 minutes every 3 to 4 hours to help with swelling. An elastic bandage should be applied from toe to knee to give stability and reduce swelling and bruising. Advice can be provided by a pharmacist to ensure correct fitting. The bandage should be firm but not tight enough to cut of circulation to your foot. Elevate the affected leg as much as possible in the first few days to decrease swelling. Pain can be dealt with by taking regular analgesics.
Complete immobilisation should be avoided for long periods because scar tissue healing will make the ligament tighter and therefore your ankle will be stiffer delaying recovery. Severe injuries of injuries taking longer to heal will benefit from physiotherapy. A physiotherapist will give you a full range of exercises to stretch and strengthen the ligaments whilst they are healing. They may use techniques such as heat, ultrasound and massage. Exercises will also be given to strengthen the surrounding muscles to give the ankle more stability.
Inadequate recovery time or inappropriate treatment can lead to reinjury. There are a few things you can do to prevent further injury. A short term solution is to strap your ankle before activities but it is more beneficial to strengthen your ankle muscles. Have an adequate warm up routine and wear shoes that support your ankle. Balancing exercises can cut your risk of spraining your ankle again. A physiotherapist can advise you on suitable exercises.
Cricketers Rotator Cuff injury November 30, 2010
Posted by Joanna Wilson in Uncategorized.Tags: bowling injury, cricket injury, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, rotator cuff injury, shoulder injury, Sporting injury, sporting injury reading, Sports injury, sports injury reading
add a comment
The shoulder joint comes under tremendous strain during any sporting activities. None more so than fast bowling cricketers. The shoulder rotates in many directions and has a great range of movement. The motion involved in over-arm bowling strains the shoulder joint and tears in the muscle can develops over time. It can start as a minor tear but with overuse can quickly develop into a major restricting injury.
The rotator cuff is made up of a group of four muscles called the subscapularis, supraspinatus, infraspinatus and teres minor. These four muscles combined are called the rotator cuff. Shoulder sport injuries to your rotator cuff are usually caused by two things – tendonitis, an inflammation of the tendon, or a tear to the muscle caused by sudden trauma.
An acute tear happens suddenly whilst doing an activity e.g. bowling a ball, when a tearing sensation is felt in the shoulder followed by pain down the arm. A chronic tear develops over a period of time
The main symptom of a rotator cuff injury is pain which limits range of movement. The pain in your shoulder will be particularly severe when the arm is raised out to the side or you try to reach behind you. The pain may radiate down the arm to the elbow and can be worse at night. The shoulder may feel weakened and simple everyday tasks like dressing will become troublesome.
Initially treatment should be using the R.I.C.E method. Rest your shoulder for a few days avoiding the activity which causes you pain. Apply ice packs to your shoulder for about 20 minutes three to four times a day to help reduce inflammation. Never apply ice directly to the skin, wrap in a towel to prevent damage to the skin. A sling may be used for a few days to help give support to the shoulder but should not be over used as the shoulder needs gentle movement to prevent stiffness. Anti inflammatory analgesics should be taken under the advice of your G.P. to help with the pain.
If symptoms persist more than 2-3 days seek help and advice from a physiotherapist. A sports injury specialist can assess your injury and set out a treatment plan. They may give you stretching exercises to do at home to relieve symptoms and strengthen muscles to prevent further injury.
Side Strain November 16, 2010
Posted by Joanna Wilson in Uncategorized.Tags: Ashes, cricket, cricket injuries, cricket injury, Phsyiotherapy, physiocare, physiotherapy, physiotherapy reading, RICE, RICE Treatment, side strain, Sporting injury, sporting injury reading, Sports injury
add a comment
 With the Ashes beginning next week, all professional cricketers involved will be hoping to be fit. One not so lucky is left handed Australian bowler Mitchell Starc who is out for four weeks with a side strain.
With the Ashes beginning next week, all professional cricketers involved will be hoping to be fit. One not so lucky is left handed Australian bowler Mitchell Starc who is out for four weeks with a side strain.
A side strain is typical in bowlers and is a tear in the internal oblique, external oblique or the transversalis fascia muscles where they attach to the bottom four ribs and affects the non-bowling arm side as a result of forcible contraction of the muscles on that side whilst they are fully stretched as the bowling arm is set for bowling.
Symptoms are sudden onset pain accompanied with swelling bruising and restricted range of movement. Depending on the severity of the tear will depend on the severity of the pain. A substantial injury will result in severe pain, extensive bruising and pain on breathing.
Treatment initially is by the R.I.C.E method. Resting for the first 72 hours is essential to prevent further damage. Ice packs should be applied regularly to help with swelling. Never apply ice directly to the skin as this will cause ice burns. A cohesive compression bandage may be applied to limit bleeding into the surrounding tissues.
Physiotherapy will help with rehabilitation. Core stretching and strengthening exercises should be begun as soon as the physiotherapist recommends. Early return to activity is needed to optimise the regeneration of the healing muscle and recovery of the flexibility and strength of the muscle.
A physiotherapist will give you exercises to help with increase of movement and trunk stability. This may be achieved with a Pilates ball and resistance bands.
Prevention of this injury will be especially difficult for professional cricketers. Ensuring adequate rest between activities and having a good warm-up regime will help. Bowlers should have a break after a certain amount of overs to prevent over use.
